Bulimia: what it is, symptoms, causes and how to support adolescents safely

Bulimia nervosa is a disorder characterized by binge eating followed by compensatory behaviors, with a significant impact on the physical and emotional health of adolescents.
Strongly associated with anxietyand self-esteem, requires early identification and specialized monitoring. 🚨
In this article, we explain what bulimia is, its symptoms and factors that contribute to its development.
What is bulimia nervosa?
Bulimia Nervosa is a serious disorder characterized by episodes of compulsion to eat followed by compensatory behaviors to avoid weight gain, such as vomiting or excessive physical exercise.
It also involves a feeling of lack of control over the act of eating.
Individuals with bulimia may have difficulty maintaining a healthy weight and have a distorted body image (weight and shape) that influences their self-assessment.
Bulimia is not just a problem with food; involves body image, self-esteem, emotion management, stressand other underlying issues. 😞
It can affect anyone, regardless of age, gender or origin.
Identifying the early symptoms of bulimia is crucial to the effectiveness of treatment and to prevent the future development of the disorder!
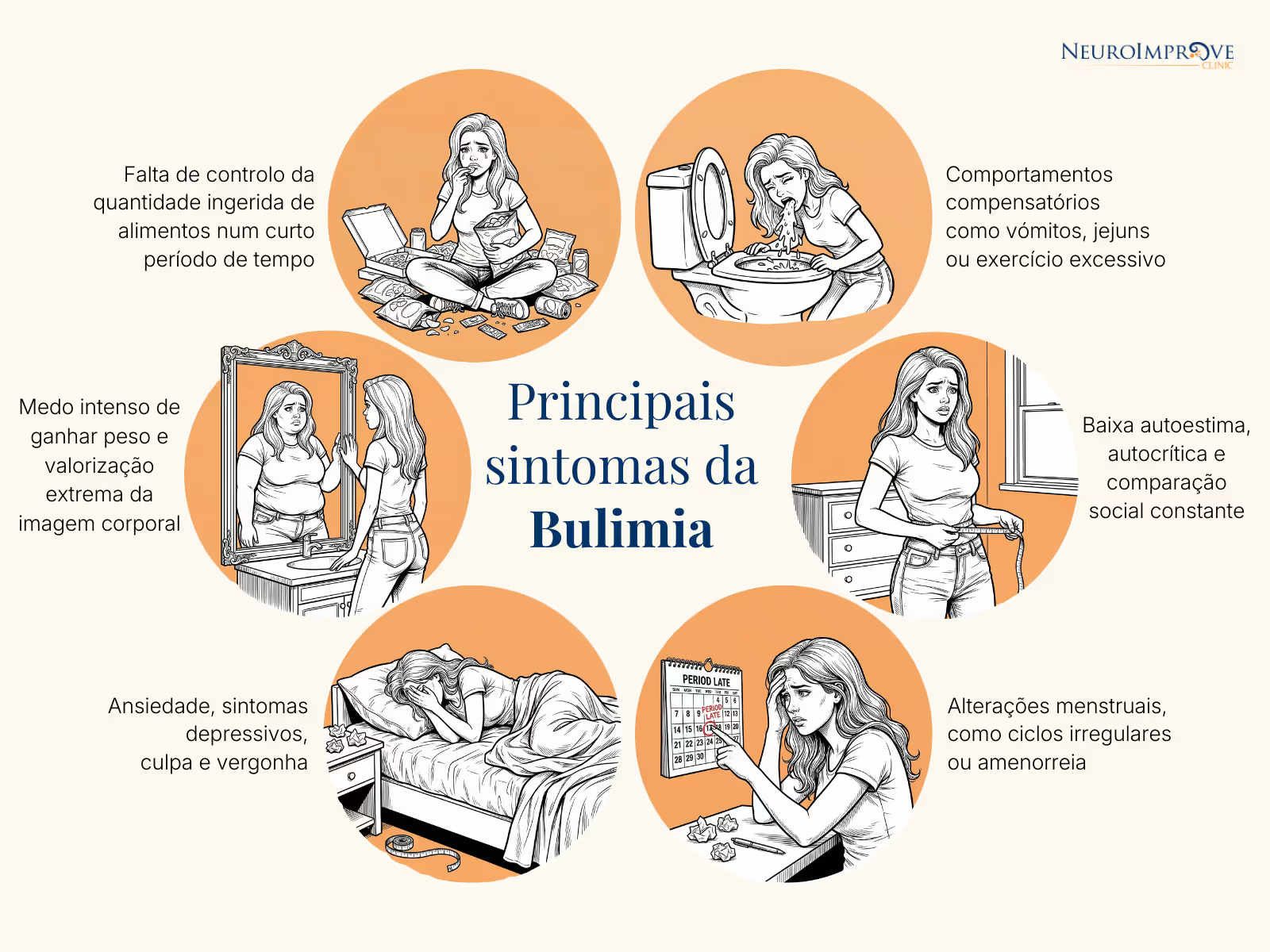
Common symptoms of bulimia
- Consume large amounts of food in a short period of time, with a feeling of loss of control.
- Perform behaviors such as vomiting, fasting or excessive exercise to compensate for food intake.
- Intense fear of gaining weight and extreme appreciation of body shape in self-image.
- Anxiety, depressive symptoms, guilt and shame; many adolescents hide their behaviors.
- Low self-esteem, self-criticism and constant social comparison.
- Menstrual changes, such as irregular cycles or amenorrhea.
Symptoms can remain hidden for months — or years — because teens with bulimia tend to be discreet, disciplined and often perform well in school, delaying diagnosis.
Why does bulimia happen? Factors that influence adolescents
Bulimia results from a combination of biological, psychological and social factors.
Among the most documented, we have:
Aesthetic pressure and social comparison: Intensive use of social networks and unrealistic beauty patterns increase body dissatisfaction and the risk of dysregulated eating behaviors.
😰 Anxiety and difficulty dealing with intense emotions: Many teens use food (or control over it) as a way to deal with stress, fear, guilt, or frustration.
🕵️ Perfectionism and high self-demand: Present especially in adolescents with high academic performance, sensitive to criticism or with difficulty accepting failures.
🧬 Family history of eating disorders or anxiety: Genetic and environmental factors increase vulnerability.
🧠 Neurobiological imbalances: Studies suggest alterations in reward circuitry and impulsivityin people with bulimia.
What is the difference from Bulimia to Anorexia?
Although bulimia and anorexia are both eating disorders, they differ mainly in the way they manifest.
Well bulimia, episodes of compulsive eating occur followed by compensatory behaviors, such as vomiting, fasting or excessive exercise, and the weight may remain within the values considered normal. 🍔🤮
Yes to Anorexia is characterized by persistent food restriction, intense fear of gaining weight and distortion of body image, often leading to a weight significantly lower than expected. 🚫🍔
While bulimia involves cycles of compulsion and compensation, anorexia focuses primarily on severe restriction.
How is bulimia nervosa diagnosed?
Clinical diagnosis should be carried out by psychologists and specialized doctors, following international criteria such as the DSM-5, which includes:
- Evaluation of eating behavior
- Analysis of emotional patterns
- History of weight and body image
- Compensatory Behaviors
- Functional and social impact
- Comorbidities (anxiety, depression, PHD, other emotional disturbances)
Medical examinations may be needed to assess physical risks, such as electrolyte imbalances and cardiac abnormalities.
Treatment: why it should be multidisciplinary
Bulimia nervosa requires specialized and integrated intervention, involving psychotherapy, medical monitoring, nutritional assessment, school monitoring and family support.
Although the treatment of bulimia requires specialized teams, many adolescents with this disorder present secondary symptomsthat benefit from neuropsychological intervention and emotional regulation, such as:
- Elevated anxiety
- Impulsivity
- Difficulty managing intense emotions
- Constant concerns with performance and image
- Low self-esteem
- Difficulty maintaining routines or school focus
We work precisely in these areas, using non-invasive approaches, such as Neurofeedbacke da Clinical Psychology.
When should parents seek help?
Early intervention is the variable that most influences recovery.
Parents should seek help when they observe:
⚠️ Abrupt changes in food pattern
⚠️ Frequent trips to the bathroom after meals
⚠️ Social isolation
⚠️ Excessive preoccupation with weight and shape
⚠️ Compulsive physical exercise
⚠️ Depressive mood, anxiety or irritability
⚠️ Signs of Extreme Perfectionism
You should never expect it to “pass by itself”. Eating disorders tend to get worse without support.
Final Considerations
A bulimia nervosais a serious eating disorder with significant emotional, physical and social impact for adolescents and families.
The earlier it is identified, the greater the chance of recovery and the lower the risk of complications.
NeuroImprove is not a substitute for specialized clinical treatment for eating disorders, but is available to support adolescents who have anxiety, emotional difficulties, impulsivity, or low self-esteemassociated with the framework.
The path can be challenging, but it should never be traveled alone. 💙
References
American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, 5th ed Text Revision (DSM-5-TR). Washington, D.C., American Psychiatric Association, 2022, pp 752.
Crone, C., Fochtmann, L. J., Attia, E., Boland, R., Escobar, J., Fornari, V., Golden, N., & Medicus, J. (2023). The American Psychiatric Association practice guideline for the treatment of patients with eating disorders. American Journal of Psychiatry, 180 (2). https://doi.org/10.1176/appi.ajp.23180001
Frank, G. K. W., Shott, M. E., & DeGuzman, M. C. (2019). The Neurobiology of Eating Disorders. Child and adolescent psychiatric clinics of North America, 28 (4), 629—640. https://doi.org/10.1016/j.chc.2019.05.007
National Institute of Mental Health (NIH), 2025. Eating Disorders. Department of Health and Human Services, National Institutes of Health. https://www.nimh.nih.gov/health/topics/eating-disorders
2021 Global Burden of Disease (GBD) [online database]. Seattle: Institute for Health Metrics and Evaluation; 2024. https://vizhub.healthdata.org/gbd-results/
We Train Brains, Strengthen Minds, Transform Lives
Schedule an appointment and see how we can help your family.
No time for a call now? Leave your details and we will get in touch:

Wonderful team, concerned, attentive and always available to help in everything.
With the passage of time, the results are being verified.
I am grateful to have met Neuroimprove and all its professionals.





